The video Head Impulse Test (vHIT) is a relatively new test that provides diagnostic and functional information about the vestibular system, specifically the vestibular ocular reflex (VOR.) The vHIT has its roots in the head impulse test (HIT), during which the evaluator quickly moves the patients head from side to side as the patient fixates on a point. The evaluator watches the patient’s eyes to verify that they remain fixated throughout the movement. If the patient is unable to maintain fixation, catch-up saccades will be observed which are indicative of a vestibular deficit. The challenge with the HIT is that, while it is possible to observe catch-up saccades after the head movement has stopped (called overt saccades), it is not possible to see catch-up saccades that occur during the head movement (covert saccades.)
With the advent of small lightweight cameras and increased computer processing power, it has become possible to develop systems that accurately record and analyze eye movement during rapid head movement. These systems are able to capture and objectively analyze both overt and covert saccades, thereby increasing the sensitivity for identifying vestibular deficits. By moving the patient’s head through the three planes of the semicircular canals (SCCs), it is possible to objectively analyze the function of the six canals and the VOR pathways. This information can then be used to make referrals, to supplement diagnostic information from other tests, and to improve treatment plans.
Brief Discussion on the Vestibulo-Ocular Reflex
A normal functioning VOR allows for visual fixation in the presence of head movement. The reflex is comprised of three components; the vestibular organs in the cochlea, the central processing mechanism, and the motor output to the eye muscles. (Fetter, 2007)
The semicircular canals and the otolith organs sense angular and linear movement, respectively. The SCCs are arranged in pairs based on the plane of activation and have a push-pull relationship. The two lateral canals are in the same plane and respond together to angular head movement. A head turn to the right, for example, results in ampullopetal endolymph flow (towards the ampulla) in the right ear, which results in an excitatory neural response, and ampullofugal endolymph flow (away from the ampulla) in the left ear, which is inhibitory. Similarly, the anterior canals and the contralateral posterior canals function in pairs. When head movements elicit an excitatory response on one side, the paired canal on the contralateral side produces and inhibitory response.
As the cochlea responds to head movement, information is sent to the central processing mechanism via the superior and inferior branches of the vestibular nerve. From the central processing mechanism, information is sent to the ocular muscles to produce reflexive eye movement in the opposite direction of the head movement but at the same velocity.
Evaluating the VOR
Traditionally, audiologists have evaluated the VOR with caloric stimulation during the VNG and with rotary chair testing. During the caloric test, warm stimulation results in ampullopetal flow of the endolymph which yields an excitatory response and nystagmus that beats toward the stimulated ear. Cool caloric stimulation results in ampullofugal endolymph flow and nystagmus that beats away from the stimulated ear. During rotary chair testing, rotating the patient to the right or left yields the same response as the head turns described earlier. There are limitations to these procedures, however.
Natural head movements in humans range from 0.1 to 10 Hz. Caloric stimulation, while it provides objective and measurable responses, evaluates the VOR at 0.003 Hz, which is much slower than natural movements. (Turning at 0.003 Hz is analogous to taking roughly four minutes to rotate 360 degrees.) Rotary chair evaluates the VOR at higher frequencies, but still only up to 0.64 Hz. This leaves much of the range of natural head movement unevaluated.
Additionally, superior branch of the vestibular nerve innervates the lateral and anterior SCCs and the inferior branch innervates the posterior SCC. If we are only looking at the function of the lateral canal with VNG and rotary chair, we lack information on the function of the inferior branch of the vestibular nerve.
Contributzion of vHIT to the VOR evaluation
Video head impulse testing fills in the gaps left by the traditional test protocols. Similar to VNG and rotary chair testing, vHIT provides information on the lateral SCCs, but it does so by assessing the system at frequencies between 3 and 6 Hz which are much more representative of natural head movements. It is also possible to perform head thrusts in each plane of the three pairs of SCCs to obtain information on all six canals as well as both branches of the vestibular nerve.
Performing vHIT
The vHIT equipment is comprised of goggles worn tightly over the eyes with one or more cameras tracking eye movement, an accelerometer and/or gyroscope to track head movement, and a computer to collect and analyze the data.

Figure 1: Interacoustics EyeSeeCam

Figure 2: Micromedical VORTEQ vHIT
Eye movement is analyzed relative to head movement as the evaluator moves the patient through a series of rapid head movements (impulses) in the plane of the semicircular canals. The three subtests are referred to by the canals evaluated – lateral, LARP (left anterior, right posterior), and RALP (right anterior, left posterior.)
During the horizontal subtest, the evaluator actively moves the patient’s head horizontally left and right in quick impulses of approximately 10 to 20 degrees while the patient fixates on a point directly in front of him or her. During RALP, the patients head is turned approximately 45 degrees to the left and impulses are performed in the plane of the right anterior and left posterior canals. The patient’s head is then turned approximately 45 degrees to the right for the LARP and impulses are made the plane of the left anterior and right posterior canals. During RALP and LARP, the patient maintains fixation on the same point in front of him or her that was used for the lateral test. Cues from the software assist the evaluator in determining if the impulses were appropriate and when a sufficient number of impulses have been recorded. Total test time is around ten minutes.
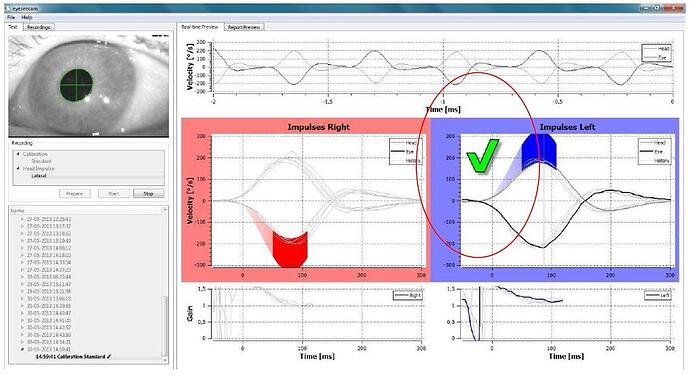
Figure 3: Interacoustics EyeSeeCam software - example of accepted impulse
After the data is collected, the software then performs an analysis of each condition and displays the results. A patient with a normal VOR will be able to maintain fixation and a patient with a deficit of the VOR system will display covert and/or overt saccades and reduced gain. The presence of catch-up saccades in each series of impulses will aid in determining which of the six canals are involved.
The examples below were obtained with the Micromedical vHIT system. The black tracings represent head movement and the green tracings represent eye movement. Figure 4 shows a normal lateral vHIT. The gain analysis is on the right side of the figure and reveals that the eye movement relative to head movement was essentially the same (gain of 1.0.)
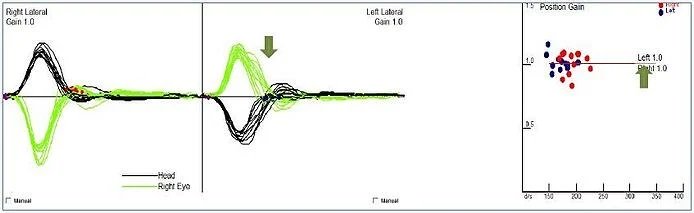
Figure 4: Micromedical vHIT results - normal lateral vHIT
Figure 5 shows the lateral vHIT results from a patient who is three years post vestibular neuritis. Compensatory saccades and reduced, asymmetrical gain is present. (The arrows indicate the catch up saccades during and after the impulse.) The reduced gain values quantify the degree to which this patient is unable to maintain fixation in the presence of head movement.
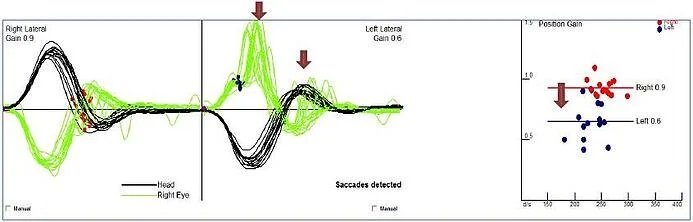
Figure 5: Abnormal left lateral vHIT
The vHIT software analyzes each condition as well as the test as a whole. Results are provided in a comprehensive report that includes normative data.
Clinical Value of vHIT
A common scenario is to use vHIT bedside or as an initial component of the vestibular assessment process. This allows the clinician to recommend the appropriate next steps to take with a patient. A quick screening of the lateral canal can be done in less than 5 minutes. If the screening is normal, additional vestibular tests will need to be performed to determine the cause of the dizziness. If the vHIT is abnormal, that information along with other screening information obtained, will help determine the specific steps needed reach a diagnosis.
Some clinics perform vHIT as part of the full vestibular workup. Performing a full vHIT evaluation adds less than ten minutes to the diagnostic appointment and is the only test that objectively evaluates the superior and anterior SCCs. Combining vHIT with VNG, ocular and cervical vestibular evoked myogenic potentials (oVEMP, cVEMP) provides information about all of the vestibular sensory receptors.
As any experienced vestibular clinician knows, VNG is not always tolerated well by patients. Patients often experience anxiety and discomfort due to discontinuing medications and limiting food intake prior to the test. Anxiety and discomfort are also common during the testing, specifically due to the dizziness and nausea that often results. Patients tend to tolerate vHIT much better as there is no need to discontinue any medications and it is significantly less likely to provoke dizziness or nausea. Since it requires very little from the patient, it can also be easily done on very young or difficult to test patients.
Since vHIT can assess the lateral canal and is tolerated better than caloric stimulation, some might ask if vHIT can replace the caloric component of the VNG assessment. This is not recommended as both tests assess the system at very different frequencies. It is also possible to have instances where vHIT is abnormal and caloric tests are normal. One study found that caloric responses may normalize in 40-60% of patients with vestibular neuritis but the head impulse test rarely normalizes. (Okinaka, Sekitani, Okazaki, Miura, & Tahara, 1993)
Petrak, Bahner, and Beck wrote an excellent article on vHIT in the September 2013 issue of the Hearing Review. Table 1 below is from that article and highlights key points about VNG, vHIT, and rotary chair testing. It is clear that each test has clear clinical value and that utilizing two or more of these tests improves the differential diagnostic process.
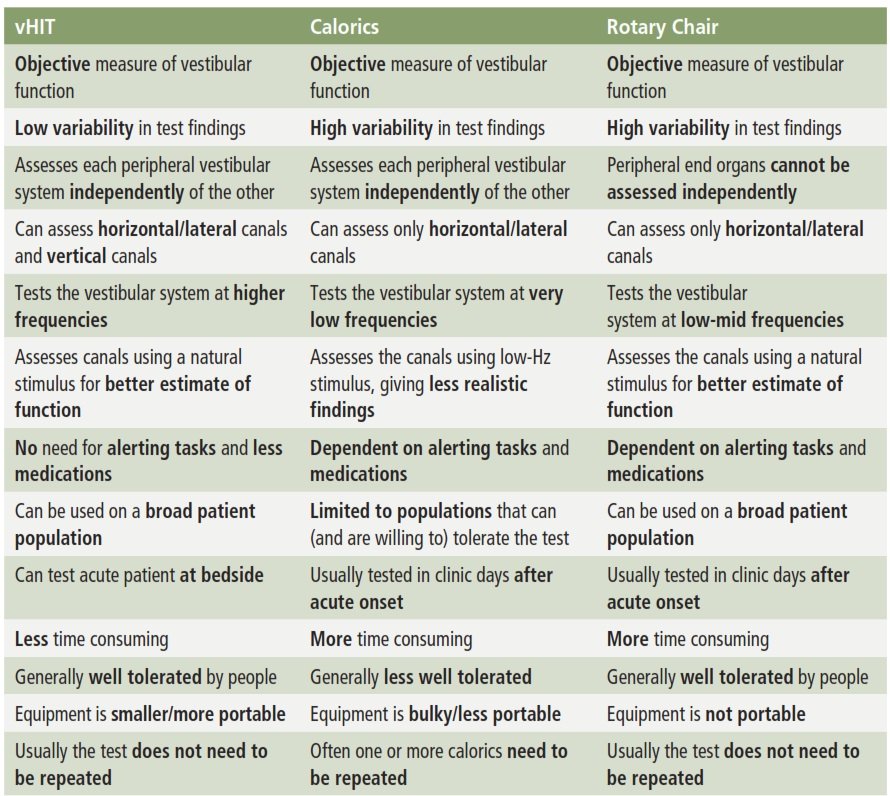
Table 1: Comparison of three vestibular tests (Petrak, Bahner, & Beck 2013)
Conclusion
The vHIT is a relatively new test that provides valuable diagnostic information about the VOR. With improvements in technology, it is now possible to record and analyze eye movements that result from head impulses. These systems are able to capture and objectively analyze both overt and covert saccades, thereby increasing the sensitivity for identifying vestibular deficits. The vHIT test is quick to perform, can be used as a screening tool or part of the diagnostic work-up, and provides information on parts of the vestibular system that previously could not objectively be evaluated. The test is also well tolerated by patients.
The vHIT is not meant to replace any existing tests. Rather, it adds to our diagnostic test battery by evaluating the vestibular system at frequencies that fall within the range of our natural head movements.
References
Fetter, M. (2007). Vestibulo-ocular reflex. Developments in Opthalmology, 40, 35-51.
MacDougall, H., Weber, K., McGarvie, L., Halmagyi, G., & Curthoys, I. (2009). The video head impulse test: Diagnostic accuracy in peripheral vestibulopathy. Neurology, 1134-1141.
Okinaka, Y., Sekitani, T., Okazaki, H., Miura, M., & Tahara, T. (1993). Progress of Caloric Response of Vestibular Neuronitis. Acta Oto-laryngologica, 18-22.
Petrak, M., Bahner, C., & Beck, D. (2013). Video Head Impulse Testing (vHIT): VOR Analysis of High Frequency Vestibular Activity. The Hearing Review, 46-50.
Interested in leveraging vHIT in your practice? Learn more about the Interacoustics EyeSeeCam today!
Learn More
About the Author
David Coffin is an audiologist and Territory Manager with e3 Diagnostics and currently oversees operations in the Northern Illinois office. He earned his Master's degree in audiology from the University of Northern Colorado in 1993 and his doctorate (Au.D.) from Salus University in 2002. Dr. Coffin has extensive experience practicing audiology in a variety of settings as well as training future generations of audiologists through his prior role teaching in a Doctor of Audiology program. His audiology passions are balance assessment and mentoring students.